Innovative Strategies for Cost-Effective Diagnosis of Barrett's Esophagus
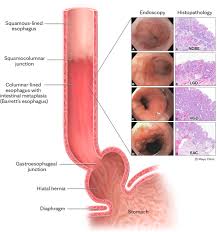
New research is investigating low-cost, non-invasive methods to diagnose Barrett's esophagus, a condition linked to a high risk of deadly esophageal cancer. Barrett's esophagus occurs when the esophageal lining is damaged due to prolonged exposure to stomach acid, with lifestyle choices like drinking and smoking contributing to its development. Current estimates suggest that 2-4% of Australians have Barrett's esophagus, primarily affecting men over 40 years old, many of whom remain unaware of their condition due to symptoms that mimic regular heartburn.
Dr. Norma Bulamu from the College of Medicine and Public Health, the lead author of the study, emphasizes the urgency of this research: "In most industrialized countries, including Australia, the incidence of esophageal cancers has increased fivefold in the past 40 years, with almost all these cancers arising from underlying Barrett's esophagus. This condition is clinically significant because individuals with Barrett's esophagus are at a heightened risk of developing esophageal cancer, which has a dismal five-year survival rate of about 20 percent. Our research aims to uncover better ways to identify and treat Barrett's esophagus to mitigate its progression to esophageal cancer and enhance patient survival rates."
Currently, diagnosis typically involves an endoscopy, an invasive procedure that examines the esophagus lining. The findings, published in the *Journal of Gastroenterology and Hepatology*, propose a multi-step strategy for Barrett's esophagus identification in the community. This approach starts with assessing patient risk levels, followed by the use of less invasive devices, and concludes with endoscopy only when necessary.
One promising device under consideration is a non-endoscopic, pill-sized instrument that collects esophageal cells, which can then be retrieved via a string for testing. However, such devices are not yet available in Australia. Dr. Bulamu notes, "Currently, there is no routine screening for Barrett's esophagus. Identification is opportunistic, limited to endoscopy, which is invasive for patients and costly for the healthcare system. Implementing a multi-step strategy is generally more economical than immediately resorting to endoscopy. The integration of less-invasive non-endoscopic devices with risk assessments could lead to an effective and cost-efficient screening method."
Senior researcher Professor David Watson adds that the study also evaluated blood-based screening tools, which were found to increase costs without significantly enhancing diagnostic accuracy. For blood tests to be viable, they need to demonstrate significantly higher sensitivity and specificity or be offered at a lower price point. Professor Watson states, "If our approach can be successfully implemented in clinics, it could facilitate screening, enabling the identification of patients with Barrett's esophagus for regular surveillance. This would allow for earlier diagnosis and treatment, particularly for those at increased risk of esophageal cancer."
While the research shows promise, the team acknowledges some limitations and suggests that further studies are needed to assess quality of life benefits and survival rates associated with early identification of esophageal cancer. Dr. Bulamu's work is supported by a Cancer Council South Australia Beat Cancer Early Career Research Fellowship.
Story Source:
Materials provided by Flinders University. The original text of this story is licensed under a Creative Commons License. Note: Content may be edited for style and length.
Journal Reference:
- Tomonori Aoki, David I. Watson, Norma B. Bulamu. Cost‐effective identification of Barrett's esophagus in the community: A first step towards screening. Journal of Gastroenterology and Hepatology, 2024; DOI: 10.1111/jgh.16762

0 Comments