Unveiling the Long-Term Dynamics of Stem Cells Post-Transplant
For the first time, scientists have tracked the fate of stem cells decades after a transplant, shedding light on a medical procedure that has remained enigmatic for over 50 years. Researchers from the Wellcome Sanger Institute, in collaboration with the University of Zurich, mapped the behavior of stem cells in recipients' bodies up to three decades post-transplant. This groundbreaking study, published on October 30 in *Nature* and partially funded by Cancer Research UK, reveals that stem cell transplants from older donors often yield significantly fewer surviving vital stem cells — ten times fewer, in fact — compared to transplants from younger donors.
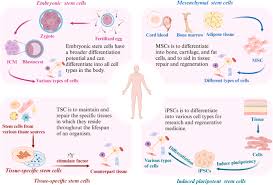
The findings are crucial, especially since over a million people are diagnosed with blood cancer globally each year, including leukemia and lymphoma. Stem cell transplants, also known as bone marrow transplants, frequently represent the only curative option for patients. These procedures involve replacing damaged blood cells with healthy stem cells from a donor, thereby rebuilding the patient’s blood and immune system. In the UK, more than 2,000 people undergo this procedure annually. Despite being performed for over five decades, many fundamental questions about the inner workings of transplants have remained unanswered, particularly regarding the role donor age plays in transplant success.
Using advanced genome sequencing techniques, the researchers analyzed blood samples from ten donor-recipient sibling pairs, tracking changes over up to 31 years post-transplant. By examining mutations in the donor and recipient’s stem cells, they could determine how many cells survived the transplant process and continued producing new blood cells. The study found that transplants from younger donors in their 20s and 30s typically result in around 30,000 long-term surviving stem cells, compared to only 1,000 to 3,000 in older donors. This significant reduction could explain the poorer outcomes often associated with older donors, leading to reduced immunity and higher relapse risks.
Additionally, the transplant process appeared to age recipients’ blood systems by approximately 10 to 15 years compared to matched donors, primarily due to lower stem cell diversity. Surprisingly, despite the intense stress of the transplant process, stem cells acquired very few new genetic mutations as they rapidly divided to rebuild the patient’s blood, challenging previous assumptions regarding high mutation rates during transplantation.
The research also identified genetic factors that help certain stem cells thrive after transplantation, regardless of donor age. Understanding these advantages could pave the way for developing better treatments and improving transplant safety and efficacy for a broader range of patients.
Dr. Michael Spencer Chapman, the study's first author at the Wellcome Sanger Institute, emphasized the significance of tracking these changes, stating, "When you receive a transplant, it's like giving your blood system a fresh start, but what actually happens to those stem cells? Until now, we could only monitor blood counts for signs of recovery. This study traces decades of changes in a single sample, revealing how certain cell populations thrive while others diminish, ultimately shaping a patient's blood over time."
Dr. Markus Manz, senior author at the University of Zurich, noted the importance of donor age in transplant success, asserting, "While the hematopoietic stem cell system is remarkably stable over time, younger donors generally provide a larger and more diverse range of stem cells, which may be crucial for long-term recovery. We hope to explore other factors affecting long-term stem cell dynamics to optimize donor selection and recipient bone-marrow environments for better stem cell function."
Dr. Peter Campbell, another senior author at the Wellcome Sanger Institute, explained how the transplant process creates a genetic 'bottleneck' for blood and immune cells. Their new approach enables them to investigate this bottleneck phenomenon more closely, identifying opportunities for specific stem cells to thrive in the recipient's new environment. Understanding which genes help some stem cells succeed could lead to improvements in the transplant procedure, enhancing the chances of successful outcomes for patients.
Story Source:
Materials provided by Wellcome Trust Sanger Institute. The original text of this story is licensed under a Creative Commons License. Note: Content may be edited for style and length.
Journal Reference:
- Michael Spencer Chapman, C. Matthias Wilk, Steffen Boettcher, Emily Mitchell, Kevin Dawson, Nicholas Williams, Jan Müller, Larisa Kovtonyuk, Hyunchul Jung, Francisco Caiado, Kirsty Roberts, Laura O’Neill, David G. Kent, Anthony R. Green, Jyoti Nangalia, Markus G. Manz, Peter J. Campbell. Clonal dynamics after allogeneic haematopoietic cell transplantation. Nature, 2024; DOI: 10.1038/s41586-024-08128-y

0 Comments