New Insights into Ovarian Cancer Resistance to Immunotherapy
Researchers at the Icahn School of Medicine at Mount Sinai have made a groundbreaking discovery regarding ovarian cancer tumors and their ability to evade immunotherapy. In a study published in the October 30 online issue of *Cell*, the team identified how these tumors manipulate their environment to resist treatment and pinpointed a potential drug target that could help overcome this resistance.
The research employed advanced spatial genomics technology alongside preclinical animal models and tumor specimens from ovarian cancer patients to validate their findings. A significant discovery was that ovarian cancer cells produce a molecule called Interleukin-4 (IL-4), which is commonly associated with conditions like asthma and eczema. This molecule helps create a protective environment that shields the tumors from killer immune cells, rendering them resistant to immunotherapy.
A drug named dupilumab, which blocks IL-4's activity, has already received FDA approval for treating asthma and eczema. The findings from this study suggest that dupilumab, or similar drugs, could be repurposed to enhance the effectiveness of immunotherapy for ovarian cancer—a disease that has a high mortality rate, with 50 percent of patients dying within five years of diagnosis.
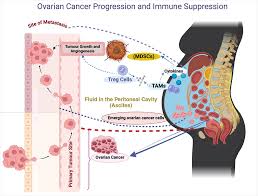
Current immunotherapy options, such as pembrolizumab that targets the PD-1 molecule, have shown effectiveness in treating other cancers like melanoma and lung cancer but have not significantly improved survival rates for ovarian cancer. One reason for this ineffectiveness is that ovarian tumors typically have fewer mutations, making it more difficult for the immune system to recognize them. Moreover, these tumors often develop barriers that prevent immune cells from infiltrating their borders.
To investigate how tumors establish these protective environments, the research team, led by Dr. Alessia Baccarini and Dr. Brian D. Brown, utilized a novel genomics technology called Perturb-map. This technique enhances traditional CRISPR screening by integrating spatial imaging, allowing for a better understanding of each gene's role in shaping the tumor environment. Their experiments revealed that removing the IL-4 gene from ovarian cancer cells made the tumors susceptible to anti-PD-1 therapy. Remarkably, even when mixed with IL-4-producing cancer cells, the IL-4-deficient cancer cells were eliminated by the immune system, showcasing the concept of intratumoral heterogeneity, which often contributes to drug resistance.
The team further tested a combination of anti-PD-1 therapy and IL-4 receptor-blocking drugs in mice with aggressive metastatic ovarian cancer, resulting in significantly extended survival rates. Additional studies demonstrated that ovarian cancer employs IL-4 to program macrophages, a type of immune cell, into protectors of the cancer cells. These IL-4-programmed macrophages inhibit T cells from effectively targeting the cancer cells. However, blocking IL-4 altered the local environment around the cancer cells, making them vulnerable to immune elimination.
To validate their findings, the researchers analyzed tumor samples from ovarian cancer patients and confirmed that the cancer cells also produced IL-4. Additionally, single-cell RNA sequencing revealed that the macrophages in these tumors displayed a strong IL-4 signature, indicating that IL-4 plays a similar role in human ovarian cancer and may contribute to the lack of benefits from immunotherapy for patients.
Dr. Brown remarked on the significance of these findings, noting that ovarian cancer had been largely considered non-responsive to existing immunotherapies. He emphasized the potential impact of simply blocking IL-4 to alter the tumor microenvironment, making these difficult-to-treat tumors more manageable. While these results are promising, the researchers stress the need for clinical trials to assess whether targeting IL-4 can enhance patient outcomes.
Given dupilumab’s existing FDA approval for asthma and eczema, there is potential for rapid clinical testing alongside immunotherapy to improve survival rates for ovarian cancer patients. Dr. Thomas Marron, Director of the Early Phase Trial Unit at Mount Sinai, is already exploring whether dupilumab can enhance anti-PD-1 immunotherapy in lung cancer patients, with several showing positive responses. Dr. Baccarini expressed optimism, stating, "Ovarian cancer is a disease that's so hard to catch early and once diagnosed, it's often too late. I am excited that these findings may make a difference in patients' lives. The IL-4 pathway is already targeted for diseases like eczema, and I am hopeful that if we target it in ovarian cancer, we can help women facing this terrible disease."
The research received support from various NIH awards and foundations, underscoring the importance of this study in advancing treatment options for ovarian cancer.
Story Source:
Materials provided by The Mount Sinai Hospital / Mount Sinai School of Medicine. The original text of this story is licensed under a Creative Commons License. Note: Content may be edited for style and length.
Journal Reference:
- Gurkan Mollaoglu, Alexander Tepper, Chiara Falcomatà, Hunter T. Potak, Luisanna Pia, Angelo Amabile, Jaime Mateus-Tique, Noam Rabinovich, Matthew D. Park, Nelson M. LaMarche, Rachel Brody, Lindsay Browning, Jia-Ren Lin, Dmitriy Zamarin, Peter K. Sorger, Sandro Santagata, Miriam Merad, Alessia Baccarini, Brian D. Brown. Ovarian cancer-derived IL-4 promotes immunotherapy resistance. Cell, 2024; DOI: 10.1016/j.cell.2024.10.006

0 Comments